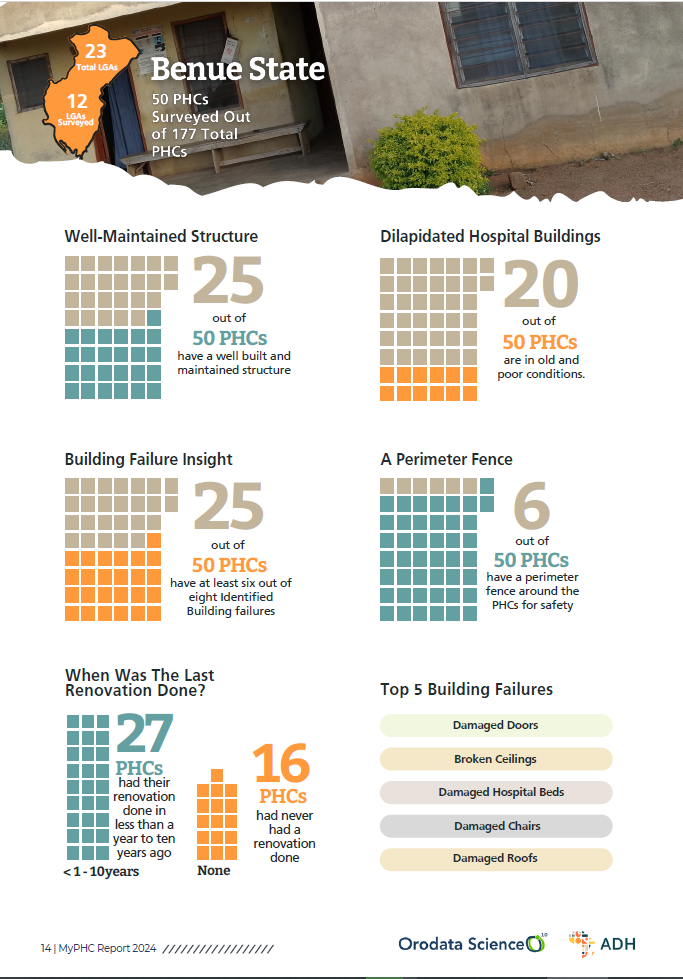
Benue State’s primary healthcare system is grappling with a myriad of challenges that threaten the delivery of quality healthcare services to its residents. A recent survey of 50 Primary Healthcare Centers (PHCs) revealed that 27 of these facilities have undergone renovation within the last decade, while 16 remain in a state of disrepair, having never been renovated. This stark reality is further compounded by the fact that half of these PHCs experience six out of eight identified building failures, including structural damage, roofing issues, and electrical faults. This compromises the safety and effectiveness of healthcare delivery, putting the lives of patients and healthcare workers at risk.
According to the Nigerian Federal Ministry of Health, “a well-functioning primary healthcare system is essential for achieving universal health coverage and improving health outcomes.” However, Benue State’s PHCs are struggling to meet this standard. Despite these infrastructure challenges, Benue’s PHCs demonstrate some strengths in terms of consulting rooms and bed availability. An impressive 46 out of 50 PHCs have consulting rooms, while 49 out of 50 PHCs have bed availability, indicating a relatively high level of essential facilities necessary for patient care and treatment.
However, the story takes a different turn when it comes to basic amenities and waste disposal infrastructure. Only 32 out of 50 PHCs have clean and functional restrooms, with waste primarily disposed of by burning or in pits/bushes, and water mainly sourced from boreholes and underground wells. This average adequacy in sanitation and water infrastructure is a far cry from the standards required for quality healthcare delivery. The World Health Organization recommends that healthcare facilities have access to safe water, sanitation, and hygiene (WASH) facilities to prevent the spread of infections and ensure patient safety.
The state’s medical equipment and supply shortages are nothing short of alarming. A paltry two out of 50 PHCs possess functional ambulances, while half of the surveyed PHCs lack at least 17 out of 18 identified medical supplies, including oxygen, PPE, stretchers, bandages, drip stands, and weighing scales. The availability of labour ward equipment is equally limited, with half of the surveyed PHCs having at least two out of five identified essential items such as delivery beds, bed pans, fetal heart rate monitors, infusion pumps, and neonatal resuscitation equipment. This severe limitation in available medical resources and labour ward equipment is a recipe for disaster, particularly in emergencies.
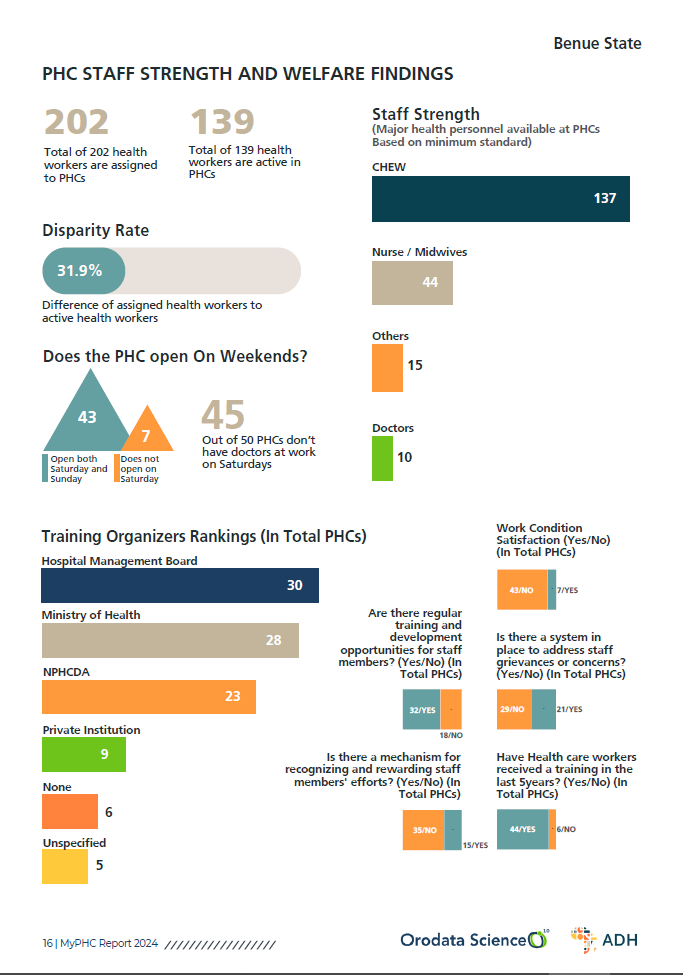
Staffing disparities and inadequate working conditions further compromise healthcare delivery. Only 139 out of 202 assigned health workers are active, resulting in a 31.19% disparity rate. The majority of PHCs lack doctor availability on weekends, and only seven out of 43 PHCs report satisfactory work conditions. This is a far cry from the recommended staff-to-patient ratio, which is essential for providing quality healthcare services. According to the Nigerian Medical Association, “a minimum of two doctors per 10,000 population is required to provide basic healthcare services.”
Staff development and training programs are also inadequate, with only 21 PHCs having systems to address staff grievances and 32 offering regular training. This is despite the fact that continuous professional development is essential for healthcare workers to deliver high-quality patient care. The Nigerian Federal Ministry of Health recommends that healthcare workers undergo regular training and development programs to enhance their skills and knowledge.
Patient usage and community engagement are affected by financial barriers, with a 36% patient affordability rate and an estimated 459 mortality cases over the last five years. This is a clear indication that many residents are unable to access healthcare services due to financial constraints. According to the World Health Organization, “financial protection is an essential component of universal health coverage.”
Referral patterns highlight critical gaps in PHC capabilities, with 1,493 referrals primarily due to complications, anemia cases, and infrastructure inadequacies. This underscores the need for improved facilities and resources to manage complex cases. The Nigerian Federal Ministry of Health recommends that PHCs have the capacity to manage common ailments and refer complex cases to secondary and tertiary healthcare facilities.
Treatment quality and service ratings vary significantly, with 21 PHCs rated very good to good and 29 rated fair to very poor. This indicates a need for quality improvement initiatives to enhance patient outcomes. According to the Nigerian Federal Ministry of Health, “quality improvement is an essential component of healthcare delivery.”
The State’s primary healthcare system faces significant challenges that threaten the delivery of quality healthcare services. Infrastructure failures, equipment shortages, staffing disparities, inadequate working conditions, and financial barriers all contribute to a system that is struggling to meet the needs of its residents. Urgent attention is required to address these challenges and ensure that Benue State’s residents have access to safe, effective, and affordable healthcare services.
For a more detailed analysis and recommendations, download the report. [Click here]