Thirty-year-old Raliya Mousa had experienced high temperatures and excessive vomiting over the night and lost some energy. Her husband, Adamu Mousa, a peasant farmer was startled by the unexpected illness but there was no medical personnel available in the community, nor could anyone suggest a diagnosis of her condition.
The only healthcare facility for the community has been abandoned due to lack of health workers in Kwarakka village, in Tangaza Local Government Area of Sokoto State, where she lives.
According to Raliya, she had been treating herself with some herbs without medical or diagnostic instructions from any qualified medical personnel.
“I was sick and the only healthcare facility in the community has not been functional for years, so I decided to treat myself but the sickness got worse day by day,” she explained in Hausa.
“ I was having a serious fever with my stomach rumbling every minute. I was dehydrated and unconscious when I was taken to a Primary Healthcare Center in Tangaza town.
During this period, she was vomiting and stooling, and became restless at night. The family had lost all hopes she would survive the illness, says Mousa.
Her situation got worse while on admission for two days at the Tangaza PHC before she was referred to Usmanu Danfodiyo University Teaching hospital in Sokoto where she regained her health.
The poor state of health care services in Tangaza Local Government Area of the state has made many people lose their lives and many others have resorted to herbal intake or self-medication for remedies.
Binta Yau’s story is similar to that of Raliya. At an early age of her pregnancy, the 29-year-old housewife had a miscarriage due to lack of antenatal care.
“We don’t have any hospital for antenatal service. I felt sick when my pregnancy was three months. I assumed it to be the normal fever but it persisted. My husband got me some herbs which I took only for me to start bleeding after some hours,” she recalled.
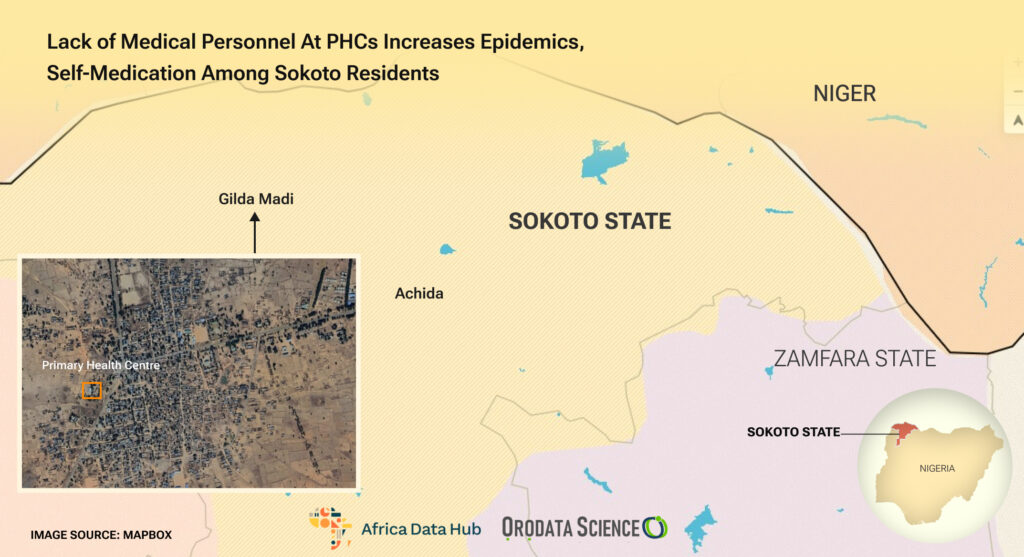
She was later rushed to a Primary Healthcare Center in Gidan Madi, Headquarters of the Local Government Council where a community Environmental Health worker suggested it could be Typhoid symptoms.
She eventually lost the pregnancy and suspected that the excess intake of some herbal substance caused her miscarriage. For years, most people from the community who fall sick use herbal medicines.
The World Health Organization (WHO) estimates that 80% of the world population relies on complementary and alternative medicines, or traditional medicine, which includes all healing practices indigenous to different cultures.
Wave of Epidemics
Illnesses such as malaria, typhoid, cholera and measles have become epidemics in several Sokoto communities according to various media reports.
Between January and July 2021, a report by the Nigeria Centre for Disease Control and Prevention showed cholera claimed no fewer than 653 lives in Nigeria, with Bauchi, Kano and Sokoto leading the list with 9,405, 5,215 and 2,651 suspected cases respectively.
In August 2021, there was an outbreak of cholera that caused havoc across some local communities in Sokoto State.
Officials in the state said no fewer than 265 cases of the disease were reported across the 13 local government councils with about 23 deaths. Tangaza was among the affected Local Government Councils.
Also in 2022, no fewer than 390 measles patients were admitted into hospitals in the state. School children were among the five deaths recorded during the year.
The NCDCP also confirmed the outbreak of Dengue fever in the state in November 2023 while over 1,000 cases of measles were from January to date.
According to the 2019 report by the World Health Organization, 20 percent of all global maternal deaths happen in Nigeria with an estimated over 600,000 maternal deaths and no less than 900,000 near-miss cases between 2005 and 2015.
Sub-Standard PHCs
While the Federal Government has recommended standards for Primary Health Centers in the country, PHCs across Sokoto State are still operating far below standard.
Checks by THE WHISTLER showed that there are no suitable wards, labour room, doctor visitation schedule, ambulance for referrals, drugs and medical equipment in some Primary healthcare facilities across the state.
This has continued to affect the wellbeing of the people who are in dire need of biomedicine remedies for their ailments.
In 2016, the Sokoto Government said it deployed 175 medical doctors, nurses and midwives to PHCs across local government areas to complement the existing health workers.
It further says the measure was to bring quality healthcare closer to the people, as well as improve immunization, maternal health and strengthen primary healthcare of the rural dwellers.
When THE WHISTLER visited some PHCs in Tangaza, most of the facilities were either abandoned or in a dilapidated state which makes the presence of medical personnel almost impossible.
Many Community Health Officials who spoke to THE WHISTLER lamented the state of the facilities and lack of qualified medical personnel. The state government was also blamed for allegedly not making enough efforts to change the situation.
In Kwarakka ward, the only health post had virtually collapsed with broken ceilings hanging down the middle of the rooms. The fence had also broken down and the building was surrounded by wild grasses.
Other healthcare facilities visited within the Tangaza community were not different.
One Doctor, 12,000 Patients
Dr. Umar Mukhtar, Chairman of Nigeria Medical Association, an umbrella body for medical personnel in Sokoto State, pointed out that lack of incentives and implementation of recommended salary structure are factors that are dissuading medical personnel from offering their services across rural communities.
Abel Martins, an Epidemiologist at the University of Abuja Teaching Hospital, also said public health facilities across the federation have continued to deteriorate. He admitted that most PHCs are faced with poor distribution of health workers, poor quality of health services, dilapidated infrastructures, and lack of supply of essential drugs as at when due.
Dr. Mukhtar said, “We’re calling on the state government to look at it critically and implement the federal structure and those doctors that are patiently working in the local government hospitals should be given special incentives.
“The World Health Organization (WHO) recommends one doctor to take charge of 600 patients but in our last briefing, here in Sokoto a single Doctor is to take charge of over 12,000 patients.”
He also revealed that many medical doctors are leaving the state for greener pastures due to better conditions of service.
“Some of our medical personnel are leaving the state for other state or Federal Government hospitals that are paying more than what the state government is paying to doctors,” he said.
He noted that the only panacea to the absence of medical personnel across the state healthcare facilities is to implement the salary structure stipulated by the Federal Government. He said this will stop “the few remaining doctors from leaving the state.”
He however called on the state government to declare a state of emergency in the health sector and improve the welfare of doctors and other health workers in the state.
We’ll Revamp PHCs – Sokoto Govt
Bello Garba, Executive Secretary, Sokoto State Primary Healthcare Agency, said the government is committed to ensuring standard healthcare services are entrench in the rural communities.
Garba, who spoke in an interview with THE WHISTLER, said the current government would revamp the Primary healthcare facilities across the state, stressing that the 2024 budget has provided more money for medical equipment and personnel.
Commissioner for Local Government and Chieftaincy Affairs, Ibrahim Dadi Adare, also revealed that the state government plans to reinstate mobile healthcare services in rural areas and free medical care targeting pregnant women and children.
He explained that rural mobile healthcare services involve deploying ambulances with teams comprising medical doctors, nurses, pharmacists, and health record specialists.
“We are going to access communities to get residents’ immediate attention and provide in-home services, while those requiring further medical attention get referrals,” he said.
This story was produced for the Frontline Investigative Program and supported by the Africa Data Hub and Orodata Science