The 2024 budgetary provision for the health sector in the state has been jacked up to 15%, which is highly commendable by Nigeria Medical Association as a way forward to efficient healthcare delivery in the state.
Enewa Peter, a 32-year-old farmer residing in Ikara community, Ado LGA, Benue State, expressed deep dissatisfaction with the inadequate infrastructure at the local primary healthcare clinic On the morning of Saturday, September 16, 2023, Peter and his family embarked on a journey to their farm to begin harvesting their crops.
“Despite experiencing a fever during her pregnancy,” Peter had attempted to manage it with local herbs. Unfortunately, the symptoms persisted. While harvesting, she unexpectedly went into labor, prompting a rush to the nearby primary healthcare clinic with the hope of safe delivery.
Upon arrival, it was discovered that the health facility had been devoid of essential child delivery tools for weeks. Additionally, there was a shortage of space and healthcare personnel, with only one government-employed staff member managing the facility. Peter endured agonizing labor for hours until her family sort for a vehicle to her a secondary health facility at Igumale.
“The prolonged pain and psychological trauma led Peter to fall into a coma during transit.” At the Igumale general hospital, the doctors and nurses worked tirelessly to revive her. Although she eventually regained consciousness, the heartbreaking outcome was the loss of her baby. Overwhelmed with grief, Peter wept inconsolably, her dream of becoming a mother after a five-year wait shattered.
According to peter “The primary health care should be prioritized as a greater proportion of the residents domiciled in rural communities in the state.”
Many others within and in other communities, face various health challenges, similar to what Peter experienced.
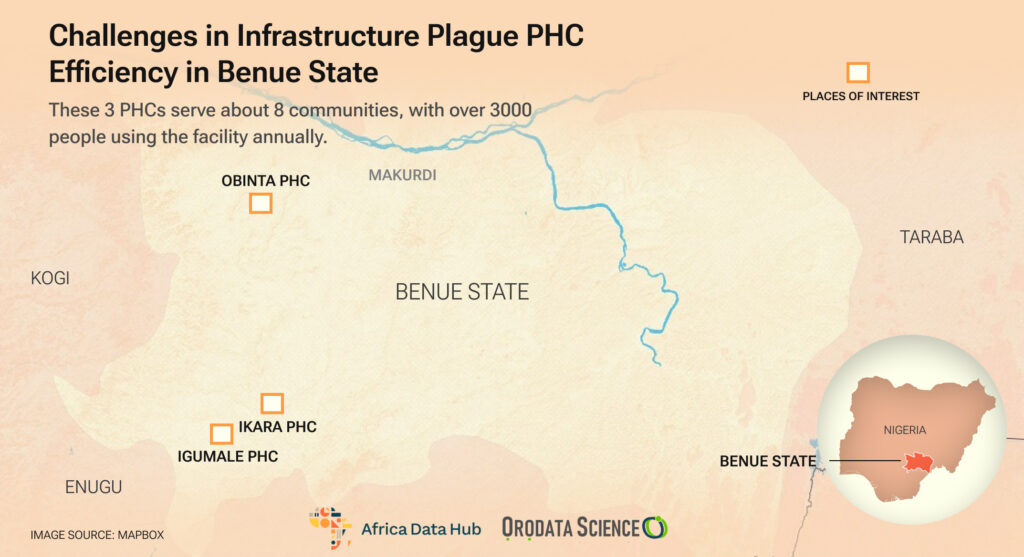
Mama Ochaiya a resident of Obinta community in Apa LGA, expressed deep concern about the deplorable condition of the health clinic outpost. The facility is marked by a severe shortage of healthcare personnel, insufficient medical supplies, and inadequate space to effectively address the community’s basic health needs.
Currently, the health outpost clinic is managed by a single individual, who is consistently overwhelmed with the workload. This shortage of staff prevents the healthcare outpost from operating round the clock, creating a significant service gap.
Furthermore, the clinic regularly experiences stockouts of essential medicines and drugs. Whenever I visit the facility, I am never able to obtain the required medications and am compelled to purchase them from a nearby chemist store. This situation underscores the critical need for urgent attention and improvements in the healthcare services provided to the community.
It is quite surprising to note that even basic medications like paracetamol are unavailable at the health facility. The situation is disheartening, and it consistently stop me from seeking medical assistance at the facility when I am sick. In my perspective, it is accurate to assert that the existing health facility does not meet the community’s expectations, to the extent that I am inclined to say there is practically no functional health outpost in this community.
John James, a lecturer at Federal College of Education at Obinta community, Apa LGA shared a similar experience as Mama Ochaiya. I hardly visit the healthcare outpost as there is barely anything to offer me as it relates to my basic healthcare needs. The health facility is often deserted of drugs and health personnel, and there is a prolonged absence of the only health personnel assigned to the facility.
This has made the community members patronize the private health facility more. The private health facility takes advantage of these lapses to charge exorbitant charges. James further said that the sorry state of the health facility calls for serious concern as locals are further exposed to health risks.
“The majority of the locals here in the community are farmers who rely so much on the PHC for their health needs, but this turns out to be the opposite” James noted.
A Clarion Call for Action
Mary Elaigwu overseeing the PHC facility at Igumale, Ado LGA has confirmed the significant infrastructural deficiencies at the primary healthcare clinics (PHCs), adversely impacting the facility’s optimal functionality. “Within this health facility, there is a shortage of space, rooms, beds, and staff, insufficient to meet the health needs of the community”. To cope with these challenges, I have to sort for additional support of volunteers, such as community health extension workers from the community. “Currently, there are only two government-employed staff members at the facility, while the remaining personnel are volunteers.
“These obstacles present significant challenges to achieving optimal service delivery, as PHCs are known to be the initial point of contact for residents in the community,” Elaigwu added.
Similarly, Mr. Godwin Okpe, the in charge of Onuebojigban health outpost expressed dissatisfaction with the prolonged neglect of the health facility. “The health outpost consists of just a single room, grossly inadequate for carrying out essential healthcare functions to meet the demands of the local population,” Okpe noted.
“Despite my efforts, as the only employed government staff alongside volunteers, the shortage of personnel remains overwhelming.” Furthermore, there is a deficiency in drug supplies to the facility, which have not been restocked for several weeks. This impedes services, forcing residents to seek drugs from private chemist stores or resort to herbal formulations. These contributing factors significantly hinder the optimal functionality of the health facility, particularly in remote and hard-to-reach communities.
He further advocates for enhanced budget allocations to the healthcare sector, particularly at the primary level to upscale the functionality of the PHCs at the grassroot.
This story was produced for the Frontline Investigative Program and supported by the Africa Data Hub and Orodata Science